The primary goal for the first phase is to allow the post-surgical trauma to resolve. Specifically, the sooner we can decrease swelling, the sooner we are able to normalize quad recruitment (a prerequisite for getting off crutches). While we appreciate that every patient wants to be off their crutches as soon as possible, it is imperative that the crutch discharge criterial is met prior to weaning off of assistive devices. These criteria are in place to ensure appropriate knee and quad function to begin walking on the newly reconstructed ligament and rushing this process will likely (and often does) lead to increased strain on the ACL. You can read more about Crutch Discharge Criteria Here. These first several weeks typically set the tone for the entire rehab process and those that prioritize modifying activity to allow swelling to resolve, consistently follow their program, and are patient with the process often do much better than those that begin walking on the new ACL before they are ready.
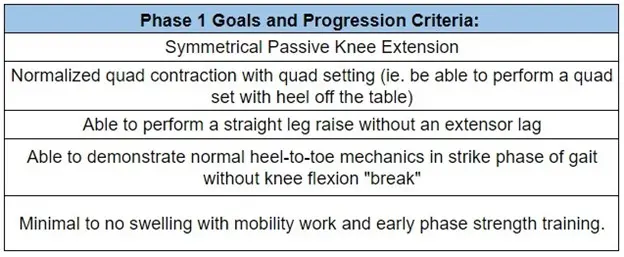
Progression Criteria for Phase 2
Phase 2 is focused primarily on establishing the training movements, specifically double leg squatting, split squats, and the hip hinge with skill and tolerance as the primary goals. Intensity is still low as we are continuing to facilitate post-surgical swelling resolution, protecting the repair, and restoring quadriceps function. At this point, we should have been able to wean off crutches, normalize gait and establish reproducibility of the designed program outside of the clinic. See Phase 2 appendix here.
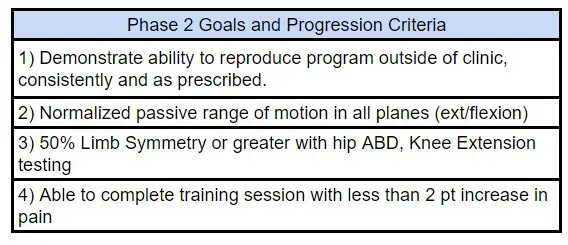
Progression Criteria For Phase 3
Phase 3 should begin to look like a true strength program with specific subjective intensity goals with anywhere from two to four training days depending on the case. We are focusing on hypertrophy, volume and strength during this phase and will begin introducing early phase plyometric skills in preparation of returning to running (see Return to Running criteria and protocol here). Around the 16 week mark we will complete our first testing session as detailed in the protocol and programming moving forward will reflect adjustments to address any suboptimal testing results.
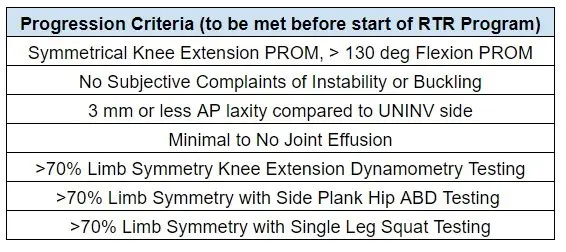
Progression Criteria For Phase 4
Assuming progression criteria has been met, this is the first block where skill work begins building in both total training volume as well as intensity. Our skill progressions will typically build off already established positions and movements (e.g. Static lunge > Rear Foot Elevated Split Squats > Bulgarian Split Squats > Bulgarian Split Squat Tempo Drill/Hops). The focus on skill development at this point is to begin moving quicker after several months of primarily lifting (note: speed and skill work can and should be completed throughout the rehab process although may be heavily modified to avoid overstressing the recent ACL reconstruction). Return to Running typically begins in this phase once criteria have been met although we will spend a few weeks re-establishing running mechanics and skills before actually running. Strength work continues to focus on building overall capacity (traditional strength programming) with an increased emphasis on more explosive lifts.
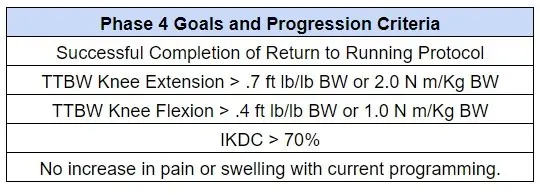
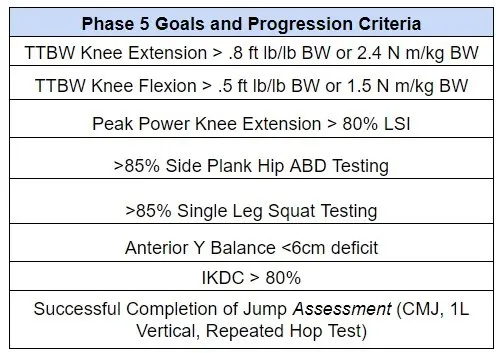
Progression Criteria For Phase 5
Phase 5 is a relatively seamless continuation of Phase 4 with the program progressing to increase speed development (acceleration, deceleration, forward sprinting) as well as conservatively introducing or progressing change of direction work. Intensity and effort emphasis on in-line speed work with skill and tolerance progressions for lower-level change of direction work. Force plate testing is usually completed at the end of this block (you can read more about our force plate testing and applications here) and programming becomes more case-specific compared to earlier phases. Common themes we see during force plate testing in this phase include slower eccentric velocity with both single leg and double leg jumping, decreased vertical jump height, increased ground contact time and asymmetrical concentric/landing strategies. It should be noted that the emphasis during this block continues to be on normalizing strength prior to normalizing jumping skills however these can, and often are, programmed simultaneously. For example, if jump height is asymmetrical in vertical jump testing and a double-digit limb symmetry strength deficit is observed, we will continue to build hip and knee strength as a priority but may also program for modified single leg jump skill development albeit with a lower time/intensity emphasis. If strength has been normalized, we will increase efforts on developing the appropriate characteristics for jump performance based on testing results. From a readiness perspective, it has been noted in other sections of this protocol that an ACL-RSI score of below 55 pts at 6 months was a predictor of decreased likelihood of returning to pre-injury levels and while it is not a specific criteria at this point of the protocol, the ACL-RSI should be complete at the beginning and end of this phase to identify early risk factors of a suboptimal outcome.
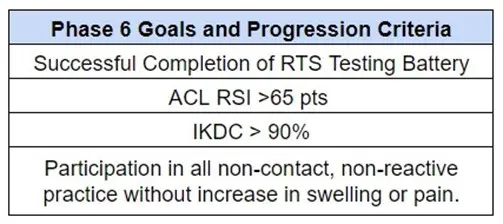
Progression Criteria For Phase 6
Phase Six is focused on primarily two things: addressing any suboptimal RTS testing results and restoring the capacities required for competitive athletics. Strength work is simplified during this phase to a primary movement, a secondary movement and one or two hypertrophy exercises with the remaining training volume dedicated towards energy system development and skill sharpening. Change of direction work, unanticipated reactive skills, and athleticism is emphasized. Towards the end of this block we should have met criteria for returning to contact although there are likely constraints in place to minimize exposures and risk. Athletes should be practicing with their team or trainers although with controls in place (i.e.. non-contact, training hours, etc.).
Progression Criteria For Return to Sport Phase
The final month is reserved for after all RTS criteria has been met with the possible exception of total workload requirements. Returning to Sport is not an inflection point but rather a spectrum where the athlete at this point should be practicing at anywhere from 50-75% of normal expectations. This last block is focused on conditioning, psychological readiness, and unanticipated reactive skills/capacity. This includes addressing any fear or confidence issues, typically through a combination of education and graded exposures. While many coaches talk about “sport-specific” training, we do not believe you can safely recreate the intensity and often chaotic nature of full intensity athletics within a clinic setting. Instead, skill work focused on improving the athlete’s confidence in their ability to do the “hard things”. Higher speed work, dual task movements, and creating a framework to improve their ability to respond to unanticipated movement is emphasized. A key factor in this phase is the establishment of an appropriate workload as briefly mentioned earlier, for returning to full in-season demands. Previous research shows a cumulative reduction in injury risk by delaying RTS from 6 months to 9 months by 84% (Grindem et al. 2016) and these months are focused on using that time to literally hit the ground running. This idea is in place to minimize an athlete spiking their workload when they are “cleared”; in other words, if they have only been training at 40-50% of their normal in-season demands, they run the risk of being undertrained and under-conditioned for a full return. Appropriate workload development and meeting all RTS testing criteria is our BEST way to minimize the modifiable risk factors for re-injury.

Sam S.
Patient
The best PT clinic out there! After my third ACL replacement I came to Nevada PT to work on my recovery. Dakota was a spectacular therapist and got me into the best shape of my life. The care they offer is far superior to the other physical therapy clinics I used in the past and I couldn't have asked for a better experience!
Read More ReviewsAleem
Patient
I cannot say enough positive things about this place. Came in with an ACL injury. I spent a few weeks working with jonathan. His evidence-based approach and motivational ability was really really inspiring. He helped me get back to normal and then some!
Read More ReviewsJamie F.
Patient
I had ACL and meniscus replacement surgery and was referred to Nevada Physical Therapy by my doctor. The owner, John, was incredibly knowledgeable, and the front staff are helpful and warm. But the real star of the show is Nick D'Agostino. His approach utilizes both physical and mental strength exercises[...]
Read More ReviewsTaylor R.
Patient
While working as a local first responder I tore my ACL several months ago. Various co-workers/friends recommended to see Jon as he has helped rehab them and yielded great results. Shortly after, I had my surgery to repair the knee and began seeing Jon. Immediately, Jon discussed his process and explained the different stages of my rehab[...]
Read More ReviewsEric W.
Patient
I saw NVPT for several months after my knee surgery. I really liked the staff (Ellie, Dakota, Britney, and Tristan). What really impressed me was how their training programs were based on the latest evidence-based research. Dakota developed a plan that allowed me to stay active while recovering so I never felt too sidelined by the injury[...]
Read More ReviewsAlex O.
Patient
Nevada Physical Therapy is by far the best physical therapy office in town. As a soccer player, injuries are a common occurrence, but Brian helped me through a particularly nasty ACL tear and it has easily been one of the best recoveries I've had [...]
Read More Reviews