One of the primary questions often asked in developing a loading protocol for a patient who has recently had anterior cruciate ligament reconstruction is: How much should we be protecting the repair versus loading it? There are multiple studies showing that mechanical loading is an important component to establishing tendon or ligament to bone homeostasis, restoring mineral density of the bone complex, stimulating healing, etc. (Wolff et al 1892; Bedi et al 2010). Bedi et al. (2010) investigated the effects of cyclical loading (2% strain x 50 repetitions daily) in surgically repaired ACLs in rats divided into three groups: immediately post-op, 4 days post-op, and 10 days post-op. They found: “At 4 weeks, the group in which delayed loading had been initiated on postoperative day 4 demonstrated a load to failure that was significantly greater than that in all other groups (13.5N +/- 4N vs 8N +/- 4N, p=0.01).” It should be noted that conflicting findings have been found in early loading versus immobilization in other animal tendon studies (Sakai et al 2000; Kamps et al 1994) and, as always, further research is needed. Additionally, several studies have demonstrated that early failure of the graft is often from anchor failure as opposed to mid-substance as demonstrated in another rat study where investigators demonstrated force to failure doubled from 2 weeks to 4 weeks post-operatively (Brophy et al 2011). It seems that, overall, mechanical loading is an important component to stimulate healing of the repaired bone to tendon or ligament site but there is still much that is unknown on what constitutes optimal loading for healing.
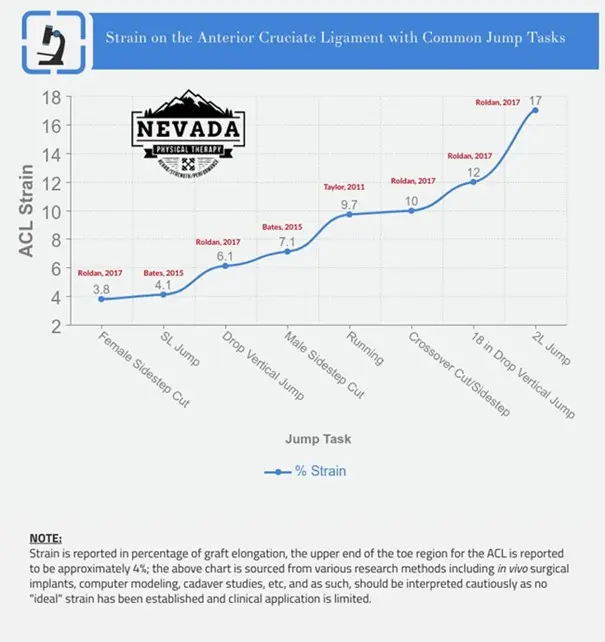
While there is very little literature establishing how much (or how little) stress is ideal to stimulate healing in a repaired anterior cruciate ligament, we do have a few dozen studies that have investigated the various forces that occur in the ACL during many rehabilitation tasks. Strain, or the lengthening of the ligament while under load, has been organized per the literature in the infographic below. What is interesting is that almost all non-plyometric movements (i.e. running, jumping, etc.) show a lower strain than seen with level ground walking (Shelbourne et al 1948). It is noteworthy that many of these studies utilized different techniques for establishing strain and stress forces such as 3-D mathematical models, cadaver modeling, motion camera analysis and surgically implanted force transducers which may limit clinical application.
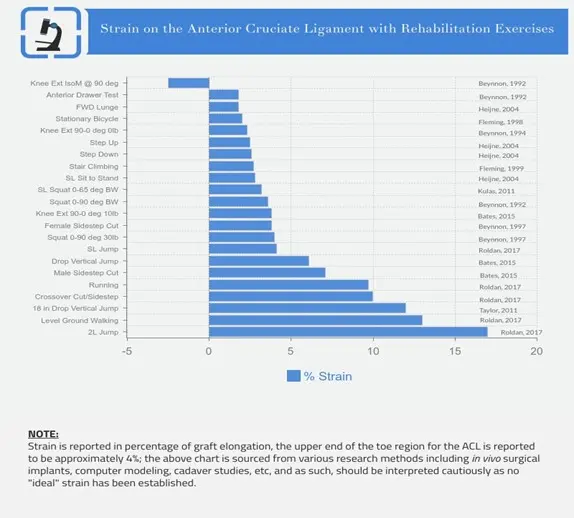
In specific reference to this protocol, we maintain limited weight bearing for the first two to 4 weeks weeks to minimize strain on the repair while the acute inflammatory process associated with surgery resolves. You can read more about phase 1 expectations here. As noted below, (Escamilla et al 2012) we may start OKC exercises such as 90 deg isometrics, 90-45 deg isotonics, etc. within the first two weeks as these appear to create minimal strain on the repair but may be helpful in restoring quad function early on. Once early phase progression criteria are met, we begin loading the knee in closed chain progressions consistent with the current evidence regarding strain profiles. This updated protocol incorporates movements like lunges, wall sits and eccentric leg press early in the post-operative phase in an attempt to minimize quad atrophy and weakness often seen in ACL reconstructed patients while minimizing excessive strain on the healing repair (Birchmieir et al 2019; Gokeler et al 2013).
The phases are broken done in more detail here, but the main takeaway from Nevada Physical Therapy’s protocol is that there are objective criteria that guide the progressions, not just time and anecdote as seen in nearly half of all currently utilized rehab programs (Burgi et al. 2019). From restoring the quadriceps to lifting to jumping and ultimately to competing, we measure and track objective criteria the entire time an athlete is with us. Once the criteria are met for jump testing, we utilize state of the art force plates to give us the ability to measure thousands of metrics on jump performance. We go into depth on our force plate testing here and we test consistently throughout the rehab program to ensure appropriate skills and capacity are restored. Quality of jumping in a sterile, i.e. controlled, environment is important, but the nature of athletics is anything but controlled. We not only measure and restore normal jumping mechanics but also create an entire skill progression based around the athlete’s unique sport demands. This includes unanticipated skill development, fatigue training protocols, and dual task or neurocognitive exposures. Jumping and landing strategies are influenced by the obvious (strength) as well as the less obvious (fear, predictive processing, cognitive load) and more.
For example, these biomechanical considerations are additionally influenced by focus of attention, e.g. performing a cognitive task while concomitantly performing a drop landing decreased knee flexion at initial contact. (Dai 2017) Frontal plane trunk position during a cutting task is influenced by whether the task is anticipated versus unanticipated. (Houck 2006) Even cueing can influence motor skill execution, retention, and transfer of that skill to novel environments, with external cues preferable to internal cues. (Wulf 2013) In athletes who had previously undergone ACL-R, external cueing (“Push off the ground as hard as you can”) resulted in >30° knee flexion at initial contact & less ground reaction force than the athletes that received an internal cue (Gokeler 2014) and similarly, a 35% increase in knee flexion at ground contact and 23% reduction in ground reaction forces when using external cueing (Favre et al 2016). External cues can be directed at the environment, or associative in nature, such as encouraging the athlete to replicate a sensation of body position felt during a recent drill. (Wulf 2013).
Anterior Cruciate Ligament injuries are one of the most commonly repaired ligaments in the body with an estimated 100-200,000 reconstructions performed each year in the United States. Having surgery does not guarantee a return to prior level of function and those who have suffered an ACL injury, unfortunately also become higher risk for a second injury with 30% of those individuals suffering a contralateral (opposite knee) ACL injury in the first few years post-reconstruction (Grindem et al 2016; Paterno et al 2014) or further, elite athletes can have as high as 50% risk of reinjury in the first postoperative year (Kaeding et al 2017). Understanding the potential contributors to re-injury risk is vital to the rehabilitation process as our goal is to get the individual or athlete back to doing what they love AND mitigating modifiable risk factors for re-injury. Non-modifiable risk factors include:
While we cannot change non-modifiable risk factors, we must do our best to address the modifiable contributions to an athlete suffering a second injury and Return to Sport testing (RTS) has become an area of research emphasis recently. This is not meant to address all the known risk factors but instead to add more depth to the Return to Sport conversation for clinicians specifically.
An important note before discussing RTS testing: there is no gold standard in place and while we have many promising studies, there are still limitations in study design, populations, etc. and the research must be interpreted both individually and as a cumulative body of knowledge. For example, in this protocol we often reference the Kyritsis et al. (2016) study, which found a 4x higher rate of reinjury for those athletes that did not clear RTS criteria, however the sensitivity (the ability of a test to correctly identify those with the ailment) and specificity (the ability of the test to correctly identify those without the ailment) was only 54% and 79% respectively. Jump testing has been a foundation assessment in RTS testing however this also is not without its criticism as Agel et al. report “this 90% rule is highly questionable because performance tests may be neither demanding nor sensitive enough to accurately identify differences between the injured and non-injured sides” (2016).
While there are limitations to the current research body, the trends continue to emerge that we need an objective criterion-based assessment to facilitate our decision-making process with clearing an athlete to return to play beyond time (42% of medical providers used time ONLY as their criteria and only 13% used an objective criteria-based assessment as described by Burgi et al, 2019 and Barber-Westin and Noyes, 2011).
One of the most debated areas in RTS testing is WHEN can the athlete safely return to play? It has been established routinely in the literature that the risk of re-injury is highest in the 6-12 months post-reconstruction (Grindem et al 2016; Kyritsis et al 2016; Schlumberger et al 2015). Grindem et al. additionally demonstrated that for every month after 6 months post-op that we delay an athlete’s return to play, the risk of reinjury decreases by 50% up until 9 months (84% total risk reduction) with no significant decrease noted beyond the nine-month mark. Similar to the previously mentioned RTS questions on validity, Capin et al. (2016) demonstrated that of the 14 athletes who cleared RTS testing, the 7 that met their RTS criteria more quickly (6.8 +/- 1.9 months) suffered second ACL injuries compared to those that met their RTS criteria later (9.5 +/1 1.9 months) and did not suffer a second ACL injury. Although a small sample pool, it is compelling information that RTS criteria cannot be used in isolation for clinical decision making in clearing an athlete to return to play. Another important consideration is the athlete’s age at the time of reconstruction. Webster et al. published a single-surgeon study showing a 6x higher rate of ipsilateral ACL injury in athletes under 20 years of age compared to controls (2014) with Magnussen et al. (2012) showing a 14.3% reinjury rate in the same age group (compared to 0.7% in those over 20 years of age) and further elaborate that 11 of the 18 reinjuries were in competitive athletes. Additionally, while MRI findings are not well correlated to outcomes when assessing sport readiness, Rabuck et al. (2016) has shown marked MRI signal changes between the 6 and 10-month mark for ACL revascularization.
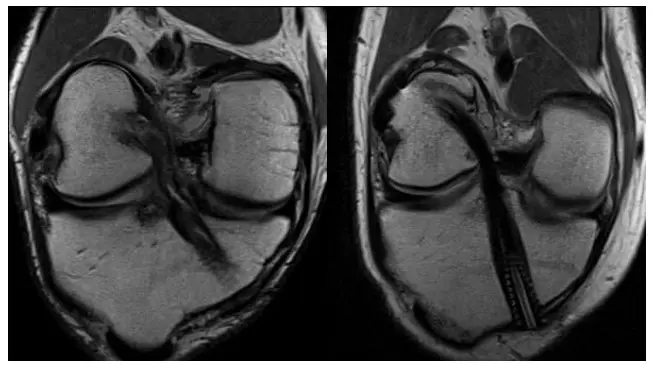
6 months vs 10 months, (image source: Rabuck et al 2016)
Nagelli and Hewett (2017) recently published an article stating that athletes “require a longer postoperative recovery period than the typically advocated 6 to 12 months to facilitate the biological recovery of the joint” with specific attention to bone-bruising which “may be recovering up to one year following ACLR and require a longer recovery period than the standard timeline according to which athletes are returning to activity”. Similar to the Rabuck study mentioned above, in regard to ACL revascularization, the researchers cite a study performed by Zaffagnini et al. (2007) that demonstrated the ACL is continuing to remodel up until 24 months after reconstruction and hamstring grafts showing a delayed remodeling phase occurring between 12-24 months in comparison to the 6–12-month timeline seen in patellar tendon autografts (Pauzenberger et al 2013). While it is unlikely that this 24-month timeline argued for by Nagelli and Hewett will be adopted in NCAA and professional athletics until additional research is done on reinjury rates on those delayed to RTS to 24 months, it does highlight that many of the early return to sport decision making criteria may not be in the best interests of the athlete and that healing (and subsequent reduction of reinjury) may be much longer than current industry standards and expectations.

Sam S.
Patient
The best PT clinic out there! After my third ACL replacement I came to Nevada PT to work on my recovery. Dakota was a spectacular therapist and got me into the best shape of my life. The care they offer is far superior to the other physical therapy clinics I used in the past and I couldn't have asked for a better experience!
Read More ReviewsAleem
Patient
I cannot say enough positive things about this place. Came in with an ACL injury. I spent a few weeks working with jonathan. His evidence-based approach and motivational ability was really really inspiring. He helped me get back to normal and then some!
Read More ReviewsJamie F.
Patient
I had ACL and meniscus replacement surgery and was referred to Nevada Physical Therapy by my doctor. The owner, John, was incredibly knowledgeable, and the front staff are helpful and warm. But the real star of the show is Nick D'Agostino. His approach utilizes both physical and mental strength exercises[...]
Read More ReviewsTaylor R.
Patient
While working as a local first responder I tore my ACL several months ago. Various co-workers/friends recommended to see Jon as he has helped rehab them and yielded great results. Shortly after, I had my surgery to repair the knee and began seeing Jon. Immediately, Jon discussed his process and explained the different stages of my rehab[...]
Read More ReviewsEric W.
Patient
I saw NVPT for several months after my knee surgery. I really liked the staff (Ellie, Dakota, Britney, and Tristan). What really impressed me was how their training programs were based on the latest evidence-based research. Dakota developed a plan that allowed me to stay active while recovering so I never felt too sidelined by the injury[...]
Read More ReviewsAlex O.
Patient
Nevada Physical Therapy is by far the best physical therapy office in town. As a soccer player, injuries are a common occurrence, but Brian helped me through a particularly nasty ACL tear and it has easily been one of the best recoveries I've had [...]
Read More Reviews